Percentage of children age 6-59 months with mild, moderate or severe anemia or with any anemia.
Coverage:
Population base: Living children born 6-59 months before the survey who stayed in the household on the night before the survey (PR file).
Time period: Current status at time of survey.
Numerators:
1) Any anemia: Number of children whose hemoglobin count is less than 11 grams per deciliter (g/dl) (hc57 in 1:3)
2) Mild anemia: Number of children whose hemoglobin count is between 10.0 and 10.9 grams per deciliter (g/dl) (hc57 = 3)
3) Moderate anemia: Number of children whose hemoglobin count is between 7.0 and 9.9 grams per deciliter (g/dl) (hc57 = 2)
4) Severe anemia: Number of children whose hemoglobin count is less than 7.0 grams per deciliter (g/dl) (hc57 = 1)
Denominator: Number of children between age 6-59 months who were measured in households selected for anemia testing who stayed in the household on the night before the survey (hv042 = 1 & hc1 in 6:59 & hc55 = 0 & hv103 = 1)
Variables: PR file.
|
hv042 |
Household selected for hemoglobin |
|
hv103 |
Slept in household |
|
hc1 |
Child's age in months |
|
hc55 |
Result of measurement – hemoglobin |
|
hc57 |
Anemia level |
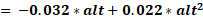
At the time of creation of a recode file, an adjustment of the hemoglobin count is made for altitude. Rather than change the cutoff points, the effective hemoglobin count is lowered as altitude increases, since oxygen is less available. The adjustment is made with the following formula:
adjust 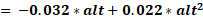
adjHb 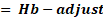 if adjust > 0
if adjust > 0
where adjust is the amount of the adjustment, alt is altitude in 1,000 feet (converted from meters by dividing by 1,000 and multiplying by 3.3), adjHb is the adjusted hemoglobin level, and Hb is the measured hemoglobin level in grams per deciliter. No adjustment is made for altitudes below 1,000 meters. Both the adjusted and unadjusted hemoglobin counts are included in the recode files.
The percentage anemic, by category, is obtained by dividing the numerators by the denominator and multiplying by 100.
Children whose mothers are not listed in the Household Questionnaire are excluded. Children who were not tested and those children whose hemoglobin values were not recorded are excluded from both the denominator and the numerators.
Children less than six months of age are not included because they have higher levels of hemoglobin at birth and just after birth and thus may distort the indication of prevalence of anemia.
People residing at higher altitudes (greater than 1,000 meters (~3,300 feet)) have higher Hb levels than those residing at sea level. This variation is due to the lower oxygen partial pressure at higher altitudes, a reduction in oxygen saturation of blood, and a compensatory increase in red cell production to ensure adequate oxygen supply to the tissues. Thus, higher altitude causes a generalized upward shift of the Hb distributions. This shift may be associated with the underdiagnosis of anemia for residents of higher altitudes when sea-level cutoffs are applied (CDC, unpublished data). Therefore, the proper diagnosis of anemia for those residing at higher altitudes requires an upward adjustment of Hb cutoffs. The values for altitude-specific adjustment of Hb are derived from data collected by the CDC Pediatric Nutrition Surveillance System on children residing at various altitudes in the mountain states. Altitude affects Hb levels throughout pregnancy in a similar way (J.N. Chatfield, unpublished data). Altitude data should always be obtained to adjust where the altitude of the dwelling is more than 1,000 meters. The DHS Program uses cluster altitude instead of altitude for each dwelling in the cluster. Note that both the adjusted and unadjusted altitude data are available in the recode files.
Centers for Disease Control and Prevention. 1998. “Recommendations to prevent and control iron deficiency in the United States.” Morbidity and Mortality Weekly Report 47 (RR-3): 1–29. https://www.cdc.gov/mmwr/pdf/rr/rr4703.pdf
Centers for Disease Control and Prevention. 1989. “Current trends CDC criteria for anemia in children and childbearing-aged women.” Morbidity and Mortality Weekly Report 38, (22): 400–404.
https://www.cdc.gov/mmwr/preview/mmwrhtml/00001405.htm
Kassebaum, N.J., R. Jasrasaria, M. Naghavi, S.K. Wulf, N. Johns, R. Lozano, M. Regan, D. Weatherall, D.P. Chou, T.P. Eisele, S.R. Flaxman, R.L. Pullan, S.J. Brooker and C.J. L. Murray. 2014. “A systematic analysis of global anemia burden from 1990 to 2010.” Blood 2014 123:615-624; doi: https://doi.org/10.1182/blood-2013-06-508325 http://www.bloodjournal.org/content/123/5/615
Nestel P. and The INACG Steering Committee. 2002. Adjusting Hemoglobin Values in Program Surveys. http://pdf.usaid.gov/pdf_docs/Pnacq927.pdf
Sullivan, K. M., Z. Mei, L. Grummer-Strawn, and I. Parvanta. 2008. “Haemoglobin Adjustments to Define Anaemia.” Tropical Medicine International Health 13(10):1267-71. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-3156.2008.02143.x
Sharman, A. 2000. Anemia testing in population-based surveys: General information and guidelines for country monitors and program managers. Calverton, Maryland USA: ORC Macro. https://dhsprogram.com/publications/publication-OD22-Other-Documents.cfm
Pullum, T., D.K. Collison, S. Namaste, and D. Garrett. 2017. Hemoglobin Data in DHS Surveys: Intrinsic Variation and Measurement Error. DHS Methodological Reports No. 18. Rockville, Maryland, USA: ICF. https://www.dhsprogram.com/publications/publication-MR18-Methodological-Reports.cfm
WHO. 2017. Nutritional Anaemias: Tools for Effective Prevention and Control. Geneva: WHO.
https://www.who.int/publications/i/item/9789241513067
WHO. 2015. The global prevalence of anaemia in 2011. https://www.who.int/publications/i/item/9789241564960
DHS-8 Tabulation plan: Table 11.12
API Indicator IDs:
CN_ANMC_C_ANY, CN_ANMC_C_MLD, CN_ANMC_C_MOD, CN_ANMC_C_SEV
WHO 100 Core Health Indicators: Anaemia prevalence in children
Percentage of women age 15-49 with mild, moderate or severe anemia or with any anemia.
Coverage:
Population base: All women age 15-49 (IR file)
Time period: Current status at time of survey
Numerators:
1) Any anemia:
· Number of non-pregnant women whose hemoglobin count is less than 12.0 grams per deciliter (g/dl) (v456 < 120)
· plus number of pregnant women whose count is less than 11.0 g/dl (v456 < 110)
2) Mild anemia:
· Number of non-pregnant women whose hemoglobin count is between 11.0 and 11.9 g/dl (v456 in 110:119)
· plus number of pregnant women whose hemoglobin count is between 10.0 and 10.9 g/dl (v456 in 100:109)
3) Moderate anemia:
· Number of non-pregnant women whose hemoglobin count is between 8.0 and 10.9 g/dl (v456 in 80:109)
· plus number of pregnant women whose hemoglobin count is between 7.0 and 9.9 g/dl (v456 in 70:99)
4) Severe anemia:
· Number of non-pregnant women whose hemoglobin count is less than 8.0 g/dl (v456<80)
· plus number of pregnant women whose hemoglobin count is less than 7.0 g/dl (v456<70)
Denominator: Number of women age 15-49 years measured for anemia in households selected for anemia testing (v042 = 1 and v455 = 0)
Variables: IR file.
|
v042 |
Household selected for hemoglobin |
|
v455 |
Result of measurement - hemoglobin |
|
v456 |
Hemoglobin level adjusted for altitude and smoking (g/dl – 1 decimal) |
|
v005 |
Women's individual sample weight |
At the time of creation of a recode file, an adjustment of the hemoglobin count is made for altitude. Rather than change the cutoff points, the effective hemoglobin count is lowered as altitude increases, since oxygen is less available. The adjustment is made with the following formulas:
adjust 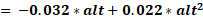
adjHb 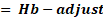 if adjust > 0
if adjust > 0
where adjust is the amount of the adjustment, alt is altitude in 1,000 feet (converted from meters by dividing by 1,000 and multiplying by 3.3), adjHb is the adjusted hemoglobin level, and Hb is the measured hemoglobin level in grams per deciliter. No adjustment is made for altitudes below 1,000 meters. Both the adjusted and unadjusted hemoglobin counts are included in the recode files.
Similarly, an adjustment is made for women who smoke (if information was collected). The adjustment is to be made in accordance with the following table:
|
Cigarettes Smoked |
Adjust Hb (g/dl) concentration by |
|
Less than 10 per day |
No adjustment |
|
10-19 per day |
-0.3 |
|
20-39 per day |
-0.5 |
|
40 or more per day |
-0.7 |
|
Unknown quantity or non-cigarettes smoking |
-0.3 |
In ever-married women samples, the data in the IR file are augmented with data from the PR file for never-married women to provide anemia prevalence estimates for all women. In ever-married samples (hv020 = 1), never-married women who are de facto residents and were tested for anemia (hv115 = 0 & hv103 = 1 & hv042 = 1 & ha55 = 0) are added to the denominator, and to the numerators if their hemoglobin levels were in the appropriate categories (ha57 in 1:3).
Added variables required for ever-married samples:
|
hv020 |
Ever-married sample |
|
hv042 |
Household selected for hemoglobin |
|
hv103 |
Slept last night |
|
ha55 |
Result of measurement – hemoglobin |
|
ha56 |
Hemoglobin level adjusted for altitude and smoking (g/dl – 1 decimal) |
|
hv005 |
Household sample weight |
The percentage anemic, by category, is obtained by dividing the numerators by the denominator and multiplying by 100.
Women who were not tested and women whose values were not recorded are excluded from both the denominator and the numerators.
Pregnancy causes an increase in blood fluid diluting somewhat the concentration of hemoglobin. Therefore, the cutoff for mild anemia is lowered for pregnant women. No adjustment is made for the cutoff values for either moderate or severe anemia. Because the availability of oxygen is less at higher altitudes (lower partial pressures) and because smoking interferes with the blood’s capacity to transfer oxygen, adjustments need to be made for both altitude and smoking.
People residing at higher altitudes (greater than 1,000 meters (~3,300 feet)) have higher Hb levels than those residing at sea level. This variation is due to the lower oxygen partial pressure at higher altitudes, a reduction in oxygen saturation of blood, and a compensatory increase in red cell production to ensure adequate oxygen supply to the tissues. Thus, higher altitude causes a generalized upward shift of the Hb distributions. This shift may be associated with the under diagnosis of anemia for residents of higher altitudes when sea-level cutoffs are applied (CDC, unpublished data). Therefore, the proper diagnosis of anemia for those residing at higher altitudes requires an upward adjustment of Hb cutoffs. The values for altitude-specific adjustment of Hb are derived from data collected by the CDC Pediatric Nutrition Surveillance System on children residing at various altitudes in the mountain states. Altitude affects Hb levels throughout pregnancy in a similar way (Chatfield, unpublished data).
The influence of cigarette smoking is similar to that of altitude; smoking increases Hb level substantially. The higher Hb of smokers is a consequence of an increased carboxyhemoglobin from inhaling carbon monoxide while smoking. Because carboxyhemoglobin has no oxygen-carrying capacity, its presence causes a generalized upward shift of the Hb distribution curves (CDC, unpublished data). Therefore, a smoking-specific adjustment to the anemia cutoff is necessary for the proper diagnosis of anemia in smokers.
The adjustment for altitude can be substantial, but the adjustment for smoking is less substantial. Thus, where no smoking information is available, no adjustment is made. However, altitude data should always be obtained to adjust where the altitude of the dwelling is more than 1,000 meters. The DHS Program uses cluster altitude instead of altitude for each dwelling in the cluster. Note that both the adjusted and unadjusted altitude data are available in the recode files.
The World Health Organization recommends slightly different hemoglobin cutoffs to define anemia for non-pregnant women: mild anemia (11.0-11.9 g/dL), moderate anemia (8.0-10.9 g/dL), and severe anemia.
These indicators could be presented based on the IR file or the PR file. Using the PR file would result in a slightly larger sample size, but the IR file is chosen for consistency with other women’s indicators, and as some of the women’s characteristics used in presenting the results are only available for women with completed interviews.
Prior to February 2019, previous versions of the Guide to DHS Statistics and previous final report tables had incorrect categorization of hemoglobin levels for non-pregnant women. Previous categories were labeled as mild anemia (10.0-11.9 g/dl), moderate anemia (7.0-9.9 g/dl), and severe anemia (<7.0 g/dl), though the true categories are mild (11.0-11.9 g/dl), moderate (8.0-10.9 g/dl), and severe (<8.0 g/dl). These incorrectly categorized levels were reflected in the variables v457 and ha57 and therefore v456 and ha56 must be used instead to estimate anemia levels when using these earlier surveys. These calculations and labels were corrected in February 2019.
Centers for Disease Control and Prevention. 1998. “Recommendations to prevent and control iron deficiency in the United States.” Morbidity and Mortality Weekly Report 47 (RR-3): 1–29.
Centers for Disease Control and Prevention. 1989. “Current trends CDC criteria for anemia in children and childbearing-aged women.” Morbidity and Mortality Weekly Report 38, (22): 400–404.
Kassebaum, N.J., R. Jasrasaria, M. Naghavi, S.K. Wulf, N. Johns, R. Lozano, M. Regan, D. Weatherall, D.P. Chou, T.P. Eisele, S.R. Flaxman, R.L. Pullan, S.J. Brooker and C.J.L. Murray. 2014. “A systematic analysis of global anemia burden from 1990 to 2010.” Blood 2014 123:615-624; doi: https://doi.org/10.1182/blood-2013-06-508325 http://www.bloodjournal.org/content/123/5/615
Nestel P. and The INACG Steering Committee. 2002. Adjusting Hemoglobin Values in Program Surveys. http://pdf.usaid.gov/pdf_docs/Pnacq927.pdf
Sullivan, K. M., Z. Mei, L. Grummer-Strawn, and I. Parvanta. 2008. “Haemoglobin Adjustments to Define Anaemia.” Tropical Medicine International Health 13(10):1267-71. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-3156.2008.02143.x
Sharman, A. 2000. Anemia testing in population-based surveys: General information and guidelines for country monitors and program managers. Calverton, Maryland USA: ORC Macro. https://dhsprogram.com/publications/publication-OD22-Other-Documents.cfm
Pullum, T., D.K. Collison, S. Namaste, and D. Garrett. 2017. Hemoglobin Data in DHS Surveys: Intrinsic Variation and Measurement Error. DHS Methodological Reports No. 18. Rockville, Maryland, USA: ICF. https://www.dhsprogram.com/publications/publication-MR18-Methodological-Reports.cfm
WHO. 2017. Nutritional Anaemias: Tools for Effective Prevention and Control. Geneva: WHO.
https://www.who.int/publications/i/item/9789241513067
WHO. 2015. The global prevalence of anaemia in 2011. https://www.who.int/publications/i/item/9789241564960
WHO. 2017. Global Nutrition Monitoring Framework: Operational Guidance for Tracking Progress in Meeting Targets for 2025. http://www.who.int/nutrition/publications/operational-guidance-GNMF-indicators/en/
DHS-8 Tabulation plan: Table 11.17.1
API Indicator IDs:
AN_ANEM_W_ANY, AN_ANEM_W_MLD, AN_ANEM_W_MOD, AN_ANEM_W_SEV
SDG Indicator 2.2.3: Prevalence of anaemia in women aged 15 to 49 years, by pregnancy status (percentage)
GNMF Indicator 2: Prevalence of haemoglobin <11 g/dL in pregnant women; Prevalence of haemoglobin <12 g/dL in non-pregnant women
WHO 100 Core Health Indicators: Anaemia prevalence in women
Percentage of men age 15-49 with mild, moderate or severe anemia or with any anemia.
Coverage:
Population base: All men age 15-49 (MR file, PR file)
Time period: Current status at time of survey
Numerator:
1) Any anemia: Number of men whose hemoglobin count is less than 13.0 grams per deciliter (g/dl) (hb56 < 130)
2) Mild anemia: Number of men whose hemoglobin count is between 11.0 and 12.9 g/dl (hb56 in 110:129)
3) Moderate anemia: Number of men whose hemoglobin count is between 8.0 and 10.9 g/dl (hb56 in 80:109)
4) Severe anemia: Number of men whose hemoglobin count is less than 8.0 g/dl (hb56 < 80)
Denominator: Number of men age 15-49 measured for anemia in households selected for anemia testing (hv042 = 1 and hb55 = 0)
Variables: MR file, PR file.
|
hv042 |
Household selected for hemoglobin |
|
hb55 |
Result of measurement – hemoglobin |
|
hb56 |
Hemoglobin level adjusted for altitude and smoking (g/dl - 1 decimal) |
|
mv005 |
Household sample weight |
To calculate the anemia status for men, it is first necessary to merge the anemia test variables from the household members recode (PR file) to the men’s recode (MR file) using the cluster, household and line numbers (see Matching and Merging Datasets in Chapter 1).
At the time of creation of a recode file, an adjustment of the hemoglobin count is made for altitude. Rather than change the cutoff points, the effective hemoglobin count is lowered as altitude increases, since oxygen is less available. The adjustment is made with the following formulas:
adjust 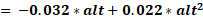
adjHb 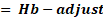 if adjust > 0
if adjust > 0
where adjust is the amount of the adjustment, alt is altitude in 1,000 feet (converted from meters by dividing by 1,000 and multiplying by 3.3), adjHb is the adjusted hemoglobin level, and Hb is the measured hemoglobin level in grams per deciliter. No adjustment is made for altitudes below 1,000 meters. Both the adjusted and unadjusted hemoglobin counts are included in the recode files.
Similarly, an adjustment is made for men who smoke (if information was collected). The adjustment is to be made in accordance with the following table:
|
Cigarettes Smoked |
Adjust Hb (g/dl) concentration by |
|
Less than 10 per day |
No adjustment |
|
10-19 per day |
-0.3 |
|
20-39 per day |
-0.5 |
|
40 or more per day |
-0.7 |
|
Unknown quantity or non-cigarettes smoking |
-0.3 |
The percentage anemic, by category, is obtained by dividing the numerators by the denominator and multiplying by 100.
Men who were not tested and men whose values were not recorded are excluded from both the denominator and the numerators.
No adjustment is made for the cutoff values for either moderate or severe anemia. Because the availability of oxygen is less at higher altitudes (lower partial pressures) and because smoking interferes with the blood’s capacity to transfer oxygen, adjustments need to be made for both altitude and smoking.
People residing at higher altitudes (greater than 1,000 meters (3,300 feet)) have higher Hb and Hct levels than those residing at sea level. This variation is due to the lower oxygen partial pressure at higher altitudes, a reduction in oxygen saturation of blood, and a compensatory increase in red cell production to ensure adequate oxygen supply to the tissues. Thus, higher altitude causes a generalized upward shift of the Hb distributions. This shift may be associated with the under diagnosis of anemia for residents of higher altitudes when sea-level cutoffs are applied (CDC, unpublished data). Therefore, the proper diagnosis of anemia for those residing at higher altitudes requires an upward adjustment of Hb cutoffs. The values for altitude-specific adjustment of Hb are derived from data collected by the CDC Pediatric Nutrition Surveillance System on children residing at various altitudes in the mountain states.
The influence of cigarette smoking is similar to that of altitude; smoking increases Hb level substantially. The higher Hb of smokers is a consequence of an increased carboxyhemoglobin from inhaling carbon monoxide while smoking. Because carboxyhemoglobin has no oxygen-carrying capacity, its presence causes a generalized upward shift of the Hb distribution curves (CDC, unpublished data). Therefore, a smoking-specific adjustment to the anemia cutoff is necessary for the proper diagnosis of anemia in smokers.
The adjustment for altitude can be substantial, but the adjustment for smoking is less substantial. Thus, where no smoking information is available, no adjustment is made. However, altitude data should always be obtained to adjust where the altitude of the dwelling is more than 1,000 meters. The DHS Program uses cluster altitude instead of altitude for each dwelling in the cluster. Note that both the adjusted and unadjusted altitude data are available in the recode files.
These indicators could be presented based on the MR file or the PR file. Using the PR file would result in a slightly larger sample size, but the MR file is chosen for consistency with other men’s indicators, and as some of the men’s characteristics used in presenting the results are only available for men with completed interviews.
Starting in DHS-8, the prevalence of mild, moderate, and severe anemia for men is shown in addition to any anemia.
Centers for Disease Control and Prevention. 1998. Recommendations to prevent and control iron deficiency in the United States. Morbidity and Mortality Weekly Report 47 (RR-3): 1–29.
Centers for Disease Control and Prevention. 1989. “Current trends CDC criteria for anemia in children and childbearing-aged women.” Morbidity and Mortality Weekly Report 38, (22): 400–404.
Nestel P. and The INACG Steering Committee. 2002. Adjusting Hemoglobin Values in Program Surveys. http://pdf.usaid.gov/pdf_docs/Pnacq927.pdf
Sullivan, K. M., Z. Mei, L. Grummer-Strawn, and I. Parvanta. 2008. “Haemoglobin Adjustments to Define Anaemia.” Tropical Medicine International Health 13(10):1267-71. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-3156.2008.02143.x
Sharman, A. 2000. Anemia testing in population-based surveys: General information and guidelines for country monitors and program managers. Calverton, Maryland USA: ORC Macro. https://dhsprogram.com/publications/publication-OD22-Other-Documents.cfm
Pullum, T., D.K. Collison, S. Namaste, and D. Garrett. 2017. Hemoglobin Data in DHS Surveys: Intrinsic Variation and Measurement Error. DHS Methodological Reports No. 18. Rockville, Maryland, USA: ICF. https://www.dhsprogram.com/publications/publication-MR18-Methodological-Reports.cfm
WHO. 2017. Nutritional Anaemias: Tools for Effective Prevention and Control. Geneva: WHO.
https://www.who.int/publications/i/item/9789241513067
DHS-8 Tabulation plan: Table 11.17.2
API Indicator IDs:
AN_ANEM_M_ANY