Percentage of children age 6-59 months who stayed in the household the night before the interview with hemoglobin lower than 8.0 g/dl.
Coverage:
Population base: Children age 6-59 months from interviewed households (PR file)
Time period: Current status at the time of the survey
Numerator: Number of de facto children age 6-59 months with a hemoglobin measurement of <8 grams per deciliter (hv042 = 1 & hv103 = 1 & hc1 in 6:59 & hc56<80)
Denominator: Number of de facto children age 6-59 months who had hemoglobin measurements obtained during the survey (hv042 = 1 & hv103 = 1 & hc1 in 6:59 & hc55=0)
Variables: HR file.
|
hv042 |
Household selected for hemoglobin |
|
hv103 |
Slept last night |
|
hc1 |
Child's age in months |
|
hc55 |
Result of measurement – hemoglobin |
|
hc56 |
Hemoglobin level adjusted for altitude |
|
hv005 |
Household sample weight |
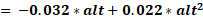
At the time of creation of a recode file, an adjustment of the hemoglobin count is made for altitude. Rather than change the cutoff points, the effective hemoglobin count is lowered as altitude increases, since oxygen is less available. The adjustment is made with the following formula:
adjust 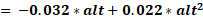
adjHb 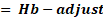 if adjust > 0
if adjust > 0
where adjust is the amount of the adjustment, alt is altitude in 1,000 feet (converted from meters by dividing by 1,000 and multiplying by 3.3), adjHb is the adjusted hemoglobin level, and Hb is the measured hemoglobin level in grams per deciliter. No adjustment is made for altitudes below 1,000 meters.
The percentage with low hemoglobin is obtained by dividing the numerator by the denominator and multiplying by 100.
Children who were not tested and those children whose values were not recorded are excluded from both the denominator and the numerators.
This is an impact indicator, as the prevalence of moderate-to-severe anemia can reflect malaria morbidity and responds to changes in the coverage of malaria interventions. Hemoglobin is measured with the HemoCue system, which requires capillary blood samples from the children in the sample.
Prevalence estimates may be biased by the seasonality of survey data collection; survey fieldwork for DHS is most often done during the dry season, while fieldwork for Malaria Indicator Surveys (MIS) is typically conducted at the end of or just after the rainy season.
An Hb concentration cut-off of less than 7.0 g/dL has been widely used to classify severe nutritional anemia, but a different cut-off, 8.0 g/dL, is used to classify malaria-related anemia, as intervention trials have shown that malaria control reduces the prevalence of moderate-to-severe anemia (below 8.0 g/dL) more so than it reduces the prevalence of any anemia (below 11.0 g/dL).
Use of anemia as a malaria indicator will be compromised by a lack of specificity, particularly in areas with low malaria transmission, given other anemia determinants such as pediatric HIV/AIDS, malnutrition and helminth infections. Even in areas of intense malaria transmission, moderate to severe anemia in young children may depend more on undernutrition than on malaria, and separating malnutrition from malaria as the cause of anemia is not possible, as the proportions will vary from population to population and cannot be known. Consequently, data must be interpreted cautiously, with consideration of the many other causes of anemia present in the survey area.
Children less than six months of age are not included because they have higher levels of hemoglobin at birth and just after birth and thus may distort the indication of prevalence of anemia.
Centers for Disease Control and Prevention. Recommendations to control and prevent iron deficiency in the United States. Morbidity and Mortality Weekly Report. Atlanta (GA): CDC (US); 1998. 47(RR-3): 1.29. https://www.cdc.gov/mmwr/pdf/rr/rr4703.pdf
Florey, L.. 2012. Anemia as an Impact Measure of ITN use Among Young Children. DHS Analytical Studies No. 31. Calverton, Maryland, USA: ICF International. https://dhsprogram.com/publications/publication-as31-analytical-studies.cfm
Korenromp E.L., J. Armstrong-Schellenberg, B. Williams, B. Nahlen, RW Snow. 2004 “Impact of malaria control on childhood anemia in Africa – a quantitative review.” Tropical Medicine International Health. 9(10): 1050-1065. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-3156.2004.01317.x
Magalhaes, R.J.S. and A.C. Clements. 2011. “Mapping the risk of anaemia in preschool-age children: the contribution of malnutrition, malaria, and helminth infections in West Africa.” PLoS medicine, 8(6), p.e1000438. http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1000438
DHS-8 Tabulation plan: Table 12.14
API Indicator IDs:
ML_HEMO_C_HL8
Household Survey Indicators for Malaria Control Indicator 13: Moderate-to-severe anemia prevalence: proportion of children aged 6-59 months with a hemoglobin measurement of <8 g/dL